
People who experience homelessness are at a significantly higher risk of suffering from poor physical and mental health. This is due to multiple, complex barriers such as stigma, health care costs, transport access, service awareness, cultural or linguistic barriers, missing documentation (e.g. Medicare card, permanent address, bank card), or lack of a regular, trusted health care provider.
In Western Sydney, we are trying to change the trend and build a health system that is equitable, affordable and welcoming to people from all backgrounds.
Street Side Medics
In response to the rising rates of homelessness in Australia, we’ve commissioned Street Side Medics, a mobile service for people experiencing homelessness in the community who find it difficult to access mainstream primary health care. The service operates from a mobile medical van staffed by skilled and dedicated volunteer GPs, junior doctors and registered nurses. Between January and March this year, these volunteers helped almost 300 patients access free health care.
All health care treatment is bulk-billed, and services include health examinations, diagnosis and treatment of medical conditions, establishing health care plans, immunisations, pathology services, nutritional advice, minor surgical procedures, and referrals to other providers. The team aim to deliver a tailored service designed to meet the individual needs of patients with a particular focus on addressing mental health, alcohol and other drugs, and chronic disease prevention and management issues.
The service operates weekly weekend clinics at:
- Blacktown, Alpha Park, Alpha St: Saturdays 3:45pm-5:45pm
- Parramatta, Prince Alfred Square, 353D Church St: Sundays 5:00pm-7:00pm
Find out more on the Street Side Medics website or call (02) 8324 7531.
Mental Health and Homelessness
Homelessness and mental health come hand-in-hand and can create a vicious cycle in which a person with insecure housing arrangements struggles to access mental health services due to multiple barriers, their mental health deteriorates, which then becomes an additional barrier to them trusting the system and accessing support.
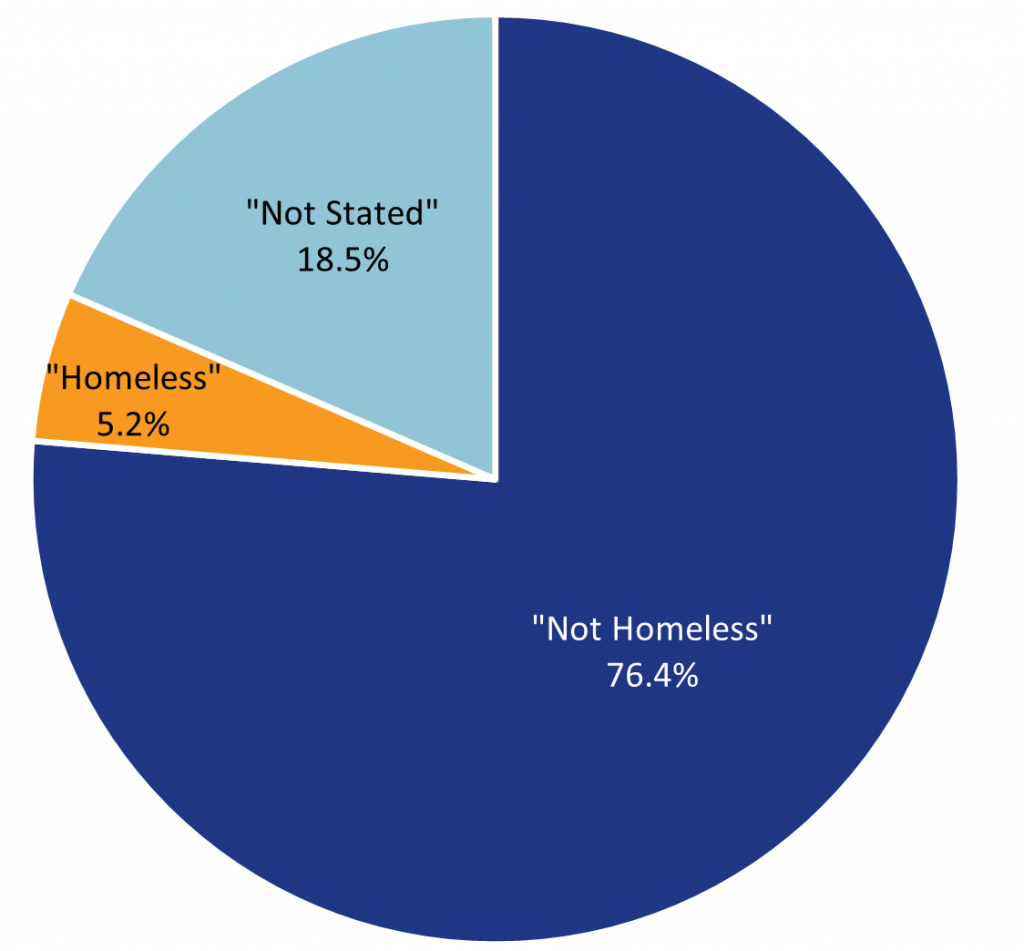
Three-quarters of clients that attended specialist state-funded mental health services in Western Sydney between July 2016 and May 2023 declared they were “not homeless”[i]. However, clients with unstable housing are harder to calculate. Although only 5% of clients stated that they were “homeless” (living in “short-term or emergency accommodation” or “sleeping rough or in non-conventional accommodation”), 18.5% of clients would not disclose their housing situation. This huge data gap means that the true scale of homelessness in Western Sydney is unclear, and, in reality, between 5.2% (2,630) to 23.6% (11,923) of mental health clients could be without stable housing.
More concerning is that 24% of mental health clients with declared housing instability have a suicide referral flag.
Mental health services also saw a large increase in stated homelessness during COVID-19. More than three times the number of clients seen during 2019/20 declared themselves homeless compared to 2018/19.
With homelessness on the rise, it is more important than ever for health professionals to consider the living status of patients and support them to connect with affordable, accessible care services.
Patients can access free mental health support without a referral from Head to Health by calling 1800 595 212. A new Head to Health Adult Mental Health Centre is opening in Parramatta this July.
[i] WentWest (2023), Client Demographics (3/4) in NMDS Mental Health dashboard, WentWest Health Intelligence Unit
Information accurate as of 22 June 2023.