
14 April 2022
Traditionally, Australian health care data has been carefully stored in silos, seldom looked at again, and even more rarely used to inform or shape health system behaviours with respect to integrated care or population health outcomes. Even before its inception as the Western Sydney Primary Health Network (WSPHN), WentWest has been a leading advocate for the way in which data from the Western Sydney community has been collected, analysed and used to deliver more cohesive primary care to the community.
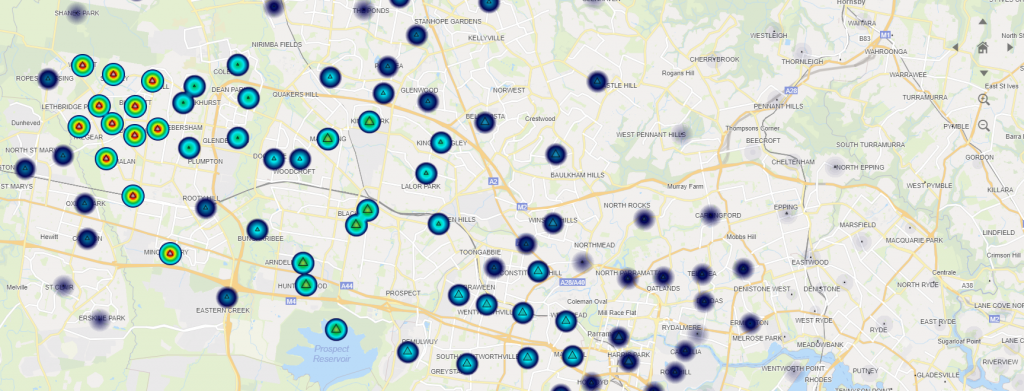
In 2016, WSPHN launched its Health Intelligence Unit (HIU) with funding secured from the Western Sydney Local Health District (WSLHD) integrated care initiative with a collaborative vision for sharing data between primary and acute settings to support patients receiving coordinated care along their health care journey. From this time, the data has been captured, interpreted and respectfully shared to inform needs assessments, policy, research and evaluation of services dedicated to improving the health and wellbeing of Western Sydney.
As capacity and capability matured, WentWest began analysing data and generating insights for the benefit of GPs to support quality improvement efforts in their practice. This saw the role of data shift from passive reporting to an important element of program development responsible for driving improved quality of care. Initially, these efforts focused in Western Sydney, but expanded across NSW through the PHN Data & Information Network, and even nationally with the Primary Health Insight (PHI) initiative based in Perth.
The power of linked primary and acute health data
WSPHN is a founding partner in the NSW Ministry of Health’s LUMOS program, a data linkage program run since 2016 to link and securely share deidentified local-level data between the WSPHN and WSLHD. This has opened the potential to develop evidence-based decision support tools for allied health professionals, GPs and specialists alike, that can coordinate care and ultimately drive improved patient outcomes. In practice, this means that when a patient has measurements taken by their local GP, they don’t have to repeat the same tests again in hospital, with the linked datasets ensuring efficient and effective management across acute and primary care settings.
Expanding data linkage into the mental health domain has the potential to dramatically improve the care of patients at risk of suicide. Today, a patient admitted to hospital following an attempted suicide, or otherwise noted to be at heightened risk of suicide, is flagged to receive follow-up contact within 48 hours of discharge, and treatment within seven days. This approach addresses a care pathway gap identified by dynamic system modelling conducted by Western Sydney University, the Sax Institute and WentWest, whereby patients would remain vulnerable due to delays between a GP referral and attendance at a specialist.
In the past, patients routinely checked for diabetes whilst admitted to hospital might not have had positive results shared with their GP. Now, through joint WSPHN and WSLHD programs such as Western Sydney Diabetes, data can be linked across primary and acute settings to track the patient journey and thereby improve their experience of care. WentWest is now working with key partners to develop a risk stratification tool for patients with relevant comorbidities to assist in early identification, and potential avoidance of preventable hospitalisations.
Most recently, WentWest has expanded the scope of its data linkage activities beyond health datasets as part of the Kids Early Years Network (KEYS) project. The KEYS Information Sharing Solution (ISS) will securely link critical de-identified information about families in distress from across primary care, acute care, Sydney Children’s Hospitals Network, the Department of Education, and the Department of Communities and Justice. Once fully operational, the project will support service providers with near real-time access to information in order to prevent families from falling between institutional gaps.
An opportunity-rich environment
The last decade has seen the public and private sectors invest significantly in improving the capture, analysis and application of data across all operational domains, and, as described above, nowhere is this truer than at WentWest.
But we are only at the start of this journey.
While our focus until now has mainly been on data supporting the delivery of health care services, interest is now shifting towards improving the capture of data representing individual and population health outcomes, with a view to informing how the health care system is funded under “value-based care”. As these efforts evolve, WentWest will continue its tradition of advocating for the respectful and sophisticated use of data and analytics as it seeks to advance the health and wellbeing of the Western Sydney community.